This comprehensive article contains critical information for fellow patients (or their relatives) with kidney disease, or at risk of kidney disease, so they can be better informed and manage their kidney problems, make better decisions with their own doctor, and minimize further complications.
Table of Contents
How do your kidneys keep you alive?
This fundamental topic on the functions of your kidneys is pivotal. You need to know how important your kidneys are, so you can value your kidneys’ health and take better care of your kidneys… to minimise the chances of kidney disease progression and complications.
So, what are the functions of your kidneys?
The main functions of your kidneys are:
- To clean the blood from wastage products produced during all processes inside the cells of your own body
- To maintain the right amount of water in your body…eliminating the excess, when needed, and conserving water when dehydrated
The kidneys do this by producing urine, which contains all the excess of toxins, electrolytes (or salts), water and medications and some environmental substances.
Urine is the by-product of filtering the blood.
Our blood gets filtered off toxins and excess of some substances by the kidneys by means of microscopic filters called glomeruli.
The filtering system is very specific and even ensures that useful substances like proteins are not lost by the kidney.
There are around 1 million of these filtering structures in one single kidney, and they work 24/7, even in your sleep.
Cleaning the blood is complex and crucial for health.
People with total kidney failure will not survive unless the kidney function is replaced through a kidney transplant or through dialysis.
Toxins, if left to accumulate in the blood, disturb many cell processes, stun the functioning of many organs and block the collaboration of many bodily systems.
The kidneys also play other important roles:
- Maintain a good balance of different salts and electrolytes in the body,
- Maintain the right level of acidity in the blood -what we call the pH, and
- Produce some hormones important for blood production (thus preventing from anaemia) and for bone health.
What happens when your kidneys do not work well?
In this section, we are going to discuss what happens when the kidneys do not work well.

Your kidneys are very valuable.
Learning what can happen if they are ill can help you put your health into perspective and make better decisions for the future.
Kidney disease and kidney failure are the consequence of damage to the microscopic filters of the kidney, that we discussed in the previous video, and they are called glomeruli.
There are many conditions that can injure the kidneys.
For example, diabetes and high blood pressure produce progressive scarring of the microfilters of the kidney and of the microscopic tubes in which the prototype urine is carried out of the kidney to later be excreted to the outside world.
Inflammation of the glomeruli, what is called glomerulonephritis, can also lead to destruction of the microfilters and microtubes in the kidneys; also ending in eventual scarring.
When the kidneys are diseased and the microfilters and microtubes are damaged, protein and/or blood might be leaked in the urine. And this is used as a laboratory marker of kidney disease.
But importantly all the functions of the kidneys get affected.
The kidneys will not be able to clean the toxins properly, leading to progressive and dangerous accumulation of toxins in the body.
The serum creatinine and urea, which are surrogate indicators of the levels of toxins in the blood, will increase in the blood.
Measuring these two substances in the blood in the laboratory helps doctors to assess the level of kidney function or the degree of kidney dysfunction, in whatever way you would like to see it.
The excess of toxins in the blood of patients can make them become very ill, lethargic, weak, nauseous or developing vomiting, with lack of appetite and excessive itch.
When the kidneys do not work well, there can be accumulation of some blood components that in the right amounts are not toxic, even healthy; but in excess, they can be even fatal, like potassium.
With high potassium, the heart can beat erratically or even stop.
There can be also fluid retention, which can range from annoyance, having heavy legs, to disturbing symptoms like causing breathlessness, or even lead to heart or respiratory failure, potentially death.
The patients can develop anaemia and bone problems, also.
The blood can also become very acidic, which can affect many processes in your body.
What are the symptoms of kidney disease? Can patients identify kidney disease at an early stage?
Now we are going to discuss whether kidney disease has symptoms that patients can identify, or not.
So, does chronic kidney disease have particular symptoms?
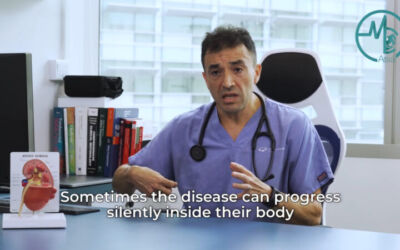
Most patients with chronic kidney disease do not experience any symptom in earlier stages of the disease. In addition, many conditions affecting the kidney do not have symptoms either.
This means patients might not be aware there is an on-going problem and they might seek medical attention quite late, which allows the kidneys to be progressively injured.
On occasions, patients might have symptoms of the original disease, which push them to see a doctor for that reason, and then the kidney problem is discovered. But that does not happen often.
Many patients’ disease is in fact discovered in late stages, once the symptoms appear.
For example, the excess of toxins in the blood of patients can make them become very ill, lethargic, weak, nauseous or developing vomiting…with lack of appetite and excessive itch. There can be fluid retention with leg swelling and breathlessness, which can endanger life.
By then, it is sometimes too late, to avoid total kidney failure.
Therefore, early detection is a critical step in the management of people who are at risk of kidney problems.
So, who is at risk of kidney problems?
Some patients might have conditions related to kidney problems like diabetes or high blood pressure; and some might have conditions highly associated with kidney disease like lupus; or have family history of kidney problems.
But from another perspective, having no symptoms in earlier stages can be good as patients can still enjoy life and perform all their activities as normal; as long as they are aware of their disease, obviously. So, they can take their precautions.
In early stages of kidney disease, patients must focus on protecting the kidneys and minimise disease progression with a better diet & lifestyle. Some might need to take medications to control their underlying conditions like high blood pressure or diabetes; or medications that are meant to provide certain protection for the kidneys.
Furthermore, an adequate monitoring strategy is pivotal, so to intervene opportunely if something is discovered, with the aim of potentially changing the outcome.
With all this, sometimes disease progression can be halted; but sometimes not, but it can be retarded, so complications appear later rather than earlier, which is beneficial.
Sometimes, renal failure can be prevented, but sometimes at least delayed, which is also beneficial.
What are the symptoms of chronic kidney disease?
Now let’s discuss what the symptoms of chronic kidney disease are.
As mentioned earlier on, chronic kidney disease, per se, has no symptoms in the earlier stages; and many conditions affecting the kidney do not have symptoms either. This means many patients might not be aware there is an on-going situation.

But when the disease progresses to a certain level, the kidneys cannot perform properly the functions that normally do; largely the cleaning of the blood and the control of water and salt, which are responsible for the majority of symptoms.
As the disease progresses, patients cannot control the water content of the body very well, so the patient starts retaining fluid in the legs. This can be annoying, making the legs feel tight and heavy and unable to wear their shoes normally or even walk with comfort.
If this is severe, the skin can break and form blisters, predisposing to skin infection, what doctors call cellulitis…worsening the problems.
If the fluid retention increases, the patient can become breathless and easily fatigued, so it is difficult to perform their normal activities.
Patients with severe fluid retention can feel breathless in the middle of the night, needing to sit up to catch up the breath or even needing to go to the emergencies department for treatment.
With excess of fluid in the body, the blood pressure of the patient goes up, and this can give the patient a headache, making him feel uneasy and can, in the long run, silently damage many organs like the brain, the heart, the eyes, and further the kidneys.
But true, if the blood pressure goes sky high, can endanger the wellbeing of many bodily organs and the life of the patient.
As the toxins levels start building in the blood, the patient can also feel very weak and very lethargic, have some nausea and vomiting, and severe itch. The patient can start losing weight and flesh.
The patient can find it difficult to concentrate in their daily activities or to remember some things, and can find it difficult to reconcile good sleep.
The patient can also become anaemic -meaning low haemoglobin or low red blood cell count.
This is caused by a deficient production by the kidney of a hormone called erythropoietin, which is involved in the production of red blood cells, which contain the haemoglobin carrying oxygen to the entire body.
Anaemia also contributes to the weakness experienced by the patient.
Occasionally, the level of anaemia can be so severe that it can impair many functions of the body as all the organs need oxygenation; and occasionally can trigger major complications like a heart attack.
To prevent anaemia, some patients must have erythropoietin injections and iron supplementation.
Patients can also have bone pains, bone deformities and even fractures because the diseased kidneys are not helping in the activation of a hormone called vitamin D, which is necessary for calcium absorption and to make the bones stronger.
In addition, patients have problems controlling the levels of phosphorus in the body, and other minerals like magnesium.
When the disease is advanced, there can be imbalances in the blood levels of many other salts or electrolytes like potassium, sodium, calcium and magnesium.
Many patients do not have symptoms, but others can have arrhythmias, that is erratic rhythms of the heart, or dizziness.
Problems of sodium, potassium, calcium and magnesium can be life-threatening, especially in advanced untreated stages.
Finally, the blood can become very acidic, which worsen many of the symptoms of the patient and impairs many organ functions inside the body.
In Francisco Kidney & Medical Centre, we aim to keep our patients well informed about their symptoms and potential complications. This can be scary for many patients. But it is ideal to be aware, so the necessary preventive measures can be put in place.
How are other organs affected by kidney disease?
So, how does the rest of the body get affected by chronic kidney disease?

With chronic kidney disease, many other organs get also affected.
The heart, vascularised organs, the brain and the nervous system are common targets.
For instance, patients with advanced chronic kidney disease, and even more, with total kidney failure, are at increased risk of heart attacks, heart failure, or erratic rhythms of the heart, or arrhythmias, that can even end-up in the heart going into stillness.
The blood pressure can go very high and this damages many other organs.
Severely increased blood pressure can precipitate a heart attack or a stroke or a bleed in the eyes.
If the potassium levels go too high, it can even make the heart stop. This can also happen with abnormalities in other electrolytes.
The bones can become fragile, leading to pain, deformities and fractures.
The muscles can also become very weak, and suffer from painful and sustained cramps.
The blood vessel can become stiff, which can cause circulation problems to many organs, then their function can be impaired.
The circulation to the heart, to the brain, to the legs, to the genitals, etc can be affected.
The nerves of the body also get affected and the patient can have loss of sensation of the skin, abnormal movement and impaired function of some organs as all organs depend on a healthy nervous system.
The skin becomes dry, which exacerbates the itch accompanying kidney disease.
And scratching predisposes to skin infection.
Organs like the liver can also not work that well with high levels of toxins, and the liver is also an important detoxifier of the body.
As the kidney disease progresses, the patient becomes more and more malnourished, losing flesh and strength.
This, together with weaker muscles and some electrolyte abnormalities, can predispose to falls and all their consequences.
If the patient becomes weaker, he becomes susceptible to transmissible infections, or he or she becomes more ill if suffering any sort of infection. Or he or she becomes more ill if suffering any sort of infection.
The mood of patients also changes, going downhill.
This might be an effect caused by the toxins or the psychological effect of knowing you have kidney disease.
In Francisco Kidney & Medical Centre, we are very aware of all the complications that kidney patients can suffer and their implications.
We provide empathetic, approachable and flexible specialist renal and medical care; because we can imagine the struggles our patients and their relatives could face in these situations. Because taking care of both the physical and mental well-being of our patients and their families is my top priority.
What are the stages of chronic kidney disease?
So, what are the stages of chronic kidney disease?
There are 5 stages of chronic kidney disease.

The 5 stages are classified according to the so-called glomerular filtration rate or GFR.
The GFR is an approximate measure of the percentage of kidney function.
In stage 1, the GFR is normal. Therefore, the kidneys clean the blood efficiently, but there is already detectable damage to the kidneys either because of protein or blood leakage in the urine, known kidney disease, for example, scars, or structural problems of the kidneys like cysts or stones.
In this stage, patients have no symptoms related to kidney dysfunction, but they might have symptoms of the original disease.
When the kidney function starts dropping progressively, meaning also the GFR starts dropping, and the injury to the kidneys progresses in intensity, chronic kidney disease moves from stage 1 to stages 2, 3, 4 and then 5.
In stages 2 to 4, typically the patient has no symptoms or only minor symptoms. Thus, it’s common to be unaware that he or she is suffering from kidney problems, unless the original disease gives them symptoms, pushing them to get checked by a doctor. For example, joint pains in lupus patients.
But those are not symptoms of chronic kidney disease.
By stage 4, many patients might have still no symptoms of kidney dysfunction or no major symptoms. However, it is advisable that patients at this stage start planning for dialysis or for a kidney transplant.
Not to start dialysis yet, but to start the planning of it. As everything in life, it is better to be prepared, to be ready and top of everything when total renal failure occurs, rather than renal failure catching the patient unguarded by surprise.
Many patients, due to natural fear for dialysis, delay the planning and end up having more complications or needing to start dialysis as an emergency.
By stage 5, many patients start having some of the symptoms of kidney failure; which were mentioned above.
As stage 5 progresses, the symptoms might be imposing on patients’ activities and well-being or might become life-threatening. In these scenarios dialysis needs to be started or a kidney transplant needs to be performed.
What is important to emphasize is that detecting chronic kidney disease early is crucial, as opportune intervention (for instance, diet and lifestyle modifications, and medications) can halt disease’s progression if they started on time.
What is uraemia and what is uraemic syndrome?
So, what is uraemic syndrome?
Uraemia is the excess of toxins in the blood, which build up because the kidneys do not filter (or clean) efficiently the blood in advanced stages of chronic kidney disease or in total kidney failure.
The excess of toxins in the blood impairs the functioning of many organs, like the brain, the liver, etc; leading to uraemic syndrome.
The uraemic syndrome is the constellation of symptoms that accompany an excess of toxins in the blood.
The patient becomes malnourished due to lack of appetite with nausea and vomiting, and due to the catabolic effect of the excess of blood toxins in the blood (which means over-consumption of body nutrients, leading to a sort of faster wear and tear of the body).
The excess of toxins also irritates the lining of the stomach and can cause bleeding from the stomach.
The mood, intellect and brain performance can be also affected.
The patient can become more anaemic, requiring very high doses of an injection called erythropoietin or maybe blood transfusions.
With severe fluid retention, with water flooding the lungs, the oxygen levels drop and they can become drowsy.
Hospitalisation might be needed, and if medical treatment is not initiated promptly, in most instances, dialysis, patients can develop life-threatening complications.
Does chronic kidney disease affect one or two kidneys?
I have been asked many times this question, if kidney disease affects one or both kidneys, by patients having the hope that one kidney is affected and the other one spare and possibly still healthy.
Unfortunately, most kidney diseases affect both kidneys, and they affect them in similar fashion, like diabetes, high blood pressure, different types of inflammation (the so called glomerulonephritis) or systemic inflammation like lupus, allergy in the kidneys (e.g. reactions to medications), urine flow obstruction that affects the urinary tubes in both sides or the bladder, polycystic kidney disease plus many other rare diseases that affect both kidneys.
But true there are diseases that can affect only one kidney like stones, tumours, accidental injuries, obstruction of the urine flow of one single kidney, a urine infection, etc. Although, true also these problems can affect the two kidneys.
The crucial matter is that many of these problems can progress to kidney failure, especially if not discovered on time or not managed adequately or by not following doctor’s recommendations. Thus, in many cases kidney failure and the need for dialysis can be prevented or at least their chances reduced if we detect them early and we treat them promptly and adequately.
It can be puzzling and difficult to understand what kidney disease means. In Francisco Kidney & Medical Centre, we do our best to answer patient’s questions and address their concerns to our best possibilities; because we can imagine the struggles our patients could face, and we care about the physical and mental well-being of our patients and their families.
How are your kidney functions assessed?
In the clinic, we use different methods to assess the degree of kidney function or kidney dysfunction, depending how you want to see it, and to confirm if your kidneys are working fine or not. Specifically, regarding how well they clean the blood.
We measure the creatinine and the urea in the blood, which indicate indirectly the levels of toxins in your body.
Higher levels of these parameters represent higher levels of toxins in the blood, indicating a lower kidney function, and that the kidneys are not cleaning the blood properly.
We also measure the glomerular filtration rate or GFR, that simplistically is an approximate measurement of the percentage of kidney function. Thus, the higher the GFR, the better the kidney function.
As part of the general assessment, we also order other tests.
An ultrasound of the kidneys, for instance.
On occasions, it helps finding the cause of the kidney problem or to detect a complication. For example, it can detect a blockage from a stone, a tumour, etc.
But the ultrasound does not measure directly the degree of kidney function, not help finding all causes of kidney problems. The fact that an ultrasound is reported as normal, it does not mean that everything is ok, still there could be an underlying problem of the kidneys, at the microscopic level, like glomerulonephritis.
But true, if the kidneys are small in the ultrasound (likely scarred), it tallies with a lower level of kidney function and usually indicates that the kidney has been injured progressively and the kidney function progressively declined through prolonged time.
In this respect, there is another useful but more invasive test, the kidney biopsy, which is a procedure using a long needle to take small pieces of the kidney for analysis under the microscope. It does not measure the capacity of cleaning of the blood, but it is in theory the best method to check the status and health of your kidneys – that is, their vitality – ; and also to find the cause of your kidney problem. However, it can be risky in patients with certain conditions and when the kidneys are too small. So, not everyone can undergo a kidney biopsy.
We also perform something we call nephritic or autoimmune screen, which consists of special blood tests, which are more detailed and expensive than routine ones. But they can be seen as an investment as they can give us peace of mind, to both doctor and patients, if they are negative; as usually point to a more severe disease. But if positive, at least a hidden process can be detected opportunely and treatment implemented promptly.
We will discuss kidney biopsy in more detail in a little while.
What do you do after a screening test shows that you might have kidney problems?
After having performed some screening tests, which could be in the form of a blood test, a urine test or an imaging test like an ultrasound of the kidneys, it is important to undergo further confirmatory tests.

I would recommend you to visit a specialist kidney doctor to arrange for that; obviously after a thorough analysis of the situation.
First of all, to confirm it. Or on the contrary, to reassure you that might not be something that significant.
Second, to assess its urgency. To differentiate if it is indeed a problem that needs to be sorted immediately or not.
Third, to assess if this could be an acute problem potentially reversible or a chronic problem, that might require different management.
Fourth, to know if the nephrologist, the urologist or their opinion combined is more relevant to provide you the best possible advice; or to check if other specialists needed to be involved in case the possibility of having a multi-organ disease.
Fifth, to identify what is the cause of kidney disease.
And sixth, based on all that, a specialist kidney doctor will suggest further diagnostic tests, will provide a treatment plan, and will advise you more accurately on its prognosis, including your chances of developing kidney failure.
Being diagnosed with kidney problems can be overwhelming, confusing and stressful. In Francisco Kidney & Medical Centre, we understand that this will bring a lot of new worries and uncertainties in your life. We aim to walk hand in hand with you.
What does it mean to have protein leaking in the urine?
Protein leaking in the urine, what we refer to as proteinuria, is typically an indicator of ongoing kidney disease, either inflammation or scarring.
You might not notice it, and it is only detected in a urine test, especially if leaking in small amounts.

There are different methods to detect protein in the urine. Rough methods are dipstick and urinalysis and they are used generally for screening or monitoring purposes.
Other methods more sensitive and specific can measure exactly the amount of protein lost in the kidney, and are per-formed after a screening test shows protein in the urine or if your kidney specialist thinks it is an important part of your assessment, for example, if you have diabetes.
Some patients with significant leaking of protein in the urine notice foamy urine, i.e. bubbles in the urine.
When it is severe, patients can develop fluid retention in many parts of the body; which is easier to perceive in the legs and in the face around the eyes, what is called nephrotic syndrome.
If you are discovered with protein in the urine you might need more thorough medical or specialist advice.
Therefore, discuss it thoroughly with your own general doctor to check if a referral with a nephrologist is necessary; especially when the cause is not known or being addressed, the amount is significant or giving you symptoms like swelling.
In Francisco Kidney & Medical Centre, we perform screening and confirmatory tests for leaking of protein in the urine, leaking of blood in the urine and for kidney disease, and we advise our patients of the following steps to follow and the likely journey, but we walk it hand in hand with them.
What are the causes of protein leaking in the urine and what it implies?
Protein leaking in the urine, what we refer to as proteinuria, is typically an indicator of ongoing kidney disease, either inflammation or scarring.

There are multiple causes of protein leaking in the urine. Sometimes, the amount of protein lost in the urine can point to certain diseases over others, and also have different implications.
But certainly, in most cases, losing protein in the urine is not normal. There are always exceptions.
In fact, proteinuria is a risk factor for kidney disease progression and a risk factor for eventual total kidney failure. This does not mean it is going to happen, but patients with proteinuria have higher chances than people without proteinuria.
Also, that risk is higher if, together with the proteinuria, there is also a leak of blood in the urine, what we call haematuria.
So, definitively, you should get it investigated, as opportune detection of a treatable cause could protect or save your kidneys- and the kidneys are vital organs.
For this, you will need to see a specialist kidney doctor.
His or her assessment might include special blood tests to detect certain causes of glomerulonephritis, which are pricier but necessary. In occasions, a kidney biopsy (which is taking a small tissue sample of the kidney) might be warranted.
But, as everything in life, there are few instances where proteinuria might not be associated with a heightened risk. Some people leak some protein during exercise, or while having fever or while having a viral infection.
These are regarded as benign because they are intermittent, transient and do not cause significant injury to the kidneys. Only specialist assessment might help you to differentiate that.
So, let’s enumerate the most common and important causes of protein leaking in the urine.
Diabetes is the most common cause of proteinuria and the most common cause of kidney failure.
Inflammation of the kidneys, what we called glomerulonephritis, follows it.
The so-called glomerulonephritis is a group of different diseases that cause proteinuria and/or haematuria, and many of them can end-up in total kidney failure, some in years or decades, but some even in days to weeks. Fortunately, the latter are not that common.
But this means, please do not leave any hint of kidney disease un-investigated and un-addressed, especially when it is painless and you might think everything is ok.
Patients with proteinuria might be treated with antiproteinuric medications, which are medications that reduce the leaking of protein in the urine by reducing the blood pressure inside the kidney, at the microscopic level.
This sort of protects the kidney to a certain level.
Treating specifically the original cause is vital, especially if glomerulonephritis, but also if diabetes or high blood pressure are the causes.
Irrespective of the cause, improvements in diet and lifestyle are important to prevent further insults and injury to the kidneys.
In Francisco Kidney & Medical Centre, we perform screening and confirmatory tests for kidney disease when we identify proteinuria, and we advise patients of the following steps to follow and the likely journey, but we will walk it hand in hand with them.
What is nephrotic syndrome?
Nephrotic syndrome is caused by some sort of inflammation of or injury to the microfilmers of the kidney (the glomeruli) making their filter pores abnormally bigger, allowing the leakage or loss of massive amounts of protein in the urine, especially albumin; typically in the realms of more than 3.5 g per day. This can be detected in a urine test.
This causes the albumin levels in the blood to drop, which has many negative effects in the body. Loss of albumin is associated with malnutrition and general weakness.
But also albumin serves like a sponge for water inside the blood vessels. So, when it reaches very low levels, water starts leaking outside the blood vessels causing swelling of the legs, face and many parts of the body like the gut. But because the water drops inside the vessels, many organs are actually dehydrated, including the kidneys, which sounds paradoxical because there is a lot of fluid retention. Patients can suffer even acute kidney failure just for that dehydration.
Together with albumin, other proteins are also lost in the urine of patients with nephrosis. These include proteins regulating the levels of cholesterol in the blood; proteins of the immune defense system (antibodies & ‘complement’); some coagulation factors; and some proteins that transport hormones like vitamin D or minerals like iron. So, patients with nephrotic syndrome can have, respectively, high cholesterol with consequent damage to the blood vessels; predisposition to infections; blood clots in different parts of the blood vessels of the venous system like the legs or the lungs; or hormonal, vitamin or mineral imbalances.
Thus, nephrotic syndrome is characterised by massive leakage of protein in the urine, low albumin in the blood, body swelling and high cholesterol, with some patients developing malnutrition, dehydration, infections and clots, and other complications.
What is the purpose of a kidney biopsy?
A kidney biopsy is a medical procedure by which a small tissue sample of one of the kidneys is taken with a fine needle. The sample is then prepared in special ways, and examined under a microscope.
This allows for detailed examination of the micro-anatomy of the kidney, revealing in most instances the cause of the kidney injury, the cause of kidney dysfunction or the cause of protein or blood leakage in the urine.
A kidney biopsy, per se, does not measure the capacity of cleaning the blood, but it is in theory the best method to check the status and health of your kidneys, and the degree of scarring of the kidneys (tissue that cannot be repaired).
A kidney biopsy can also help guide the correct treatment for your kidney condition and can help determine the prognosis or outlook of your condition. That is, the chances of disease progression.
A kidney biopsy is crucial in the management of many patients with kidney disease, but it is not a simple procedure and it is bound to complications. They are not common but they can be significant…like internal bleeding.
Therefore, patients must be assessed thoroughly by a kidney specialist.
First, to understand if a biopsy is necessary and if it needs to be performed urgently.
Second, to ensure it is safe to perform it. As it can be risky in patients with certain conditions, taking blood thinners including aspirin, and when the kidneys are too small.
So, not all people are suitable for this investigation.
Most experts agree when the kidneys are small or the damage seems to be permanent, a kidney biopsy might not be helpful also.
Many patients, in fact, refuse to have a kidney biopsy done. In many occasions, this is riskier than the biopsy itself, because the cause of the kidney problem might remain unfound, the underlying problem not treated, not monitored adequately and allowed to progress on its own, making the prognosis uncertain or not good at all.
On many occasions, with the results from the biopsy, and a proper assessment and treatment plan, kidney failure can be retarded or even avoided at all.
In Francisco Kidney & Medical Centre, we advise thoroughly on the rationale, pros and cons of performing a kidney biopsy, and we help them contrast those risks and benefits, with the risks and benefits of not doing it at all, but we respect the ultimate decision of our patients, based on their priorities.
In addition, the need or urge for a biopsy, and the risks are different for different patients.